What is glaucoma?
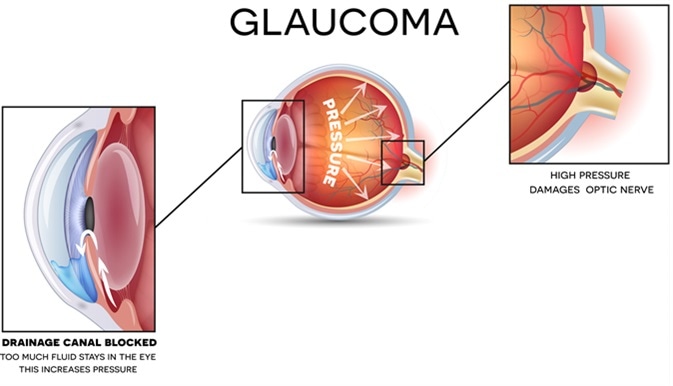
Glaucoma refers to a collection of conditions where the end result is damage to the optic nerve. At present, the main reversible risk factor is raised intraocular pressures and the vast majority of our treatments focus on reducing eye pressure as a means to reduce the risk of glaucoma progressing.
What causes glaucoma?
There are different mechanisms by which glaucoma can develop. Broadly speaking, glaucoma can be divided into open-angle and closed-angle types. The angle refers to a space between the cornea (clear window at the front of the eye) and the iris. It is important to determine whether the angle is open or closed as this will affect what the correct treatment options are.
Is glaucoma a genetic condition?
Having a first-degree relative with glaucoma increases one’s risk of developing the condition. In a very small proportion of cases, there may be a single gene that is responsible for the condition but in the majority of cases, the genetic risk is determined by a larger number of genes, each with a relatively small effect. In England, Wales and Northern Ireland, being over 40 years old with a parent, sibling, son or daughter with glaucoma, makes you eligible for a free sight test by your optician.
What are the symptoms of glaucoma?
Generally, early glaucoma may cause very few symptoms and in most patients the rate of progression is slow. Glaucoma tends to affect the peripheral vision, and this is best detected by a test called perimetry. Vision damage through glaucoma is not usually reversible so early detection is paramount so that appropriate treatment can be commenced to reduce the risk of progression.
When glaucoma results in significant visual field loss, this may have implications for eligibility to hold a UK driving license.
Rarely, patients with very high eye pressures may experience significant symptoms including eye ache or headache, blurry vision, haloes around lights and nausea/vomiting.
How do you test for glaucoma?
Diagnosing glaucoma involves a number of different tests:
Examination of the optic disc (the front part of the optic nerve). Glaucoma may cause characteristic changes in the appearance of the optic disc.
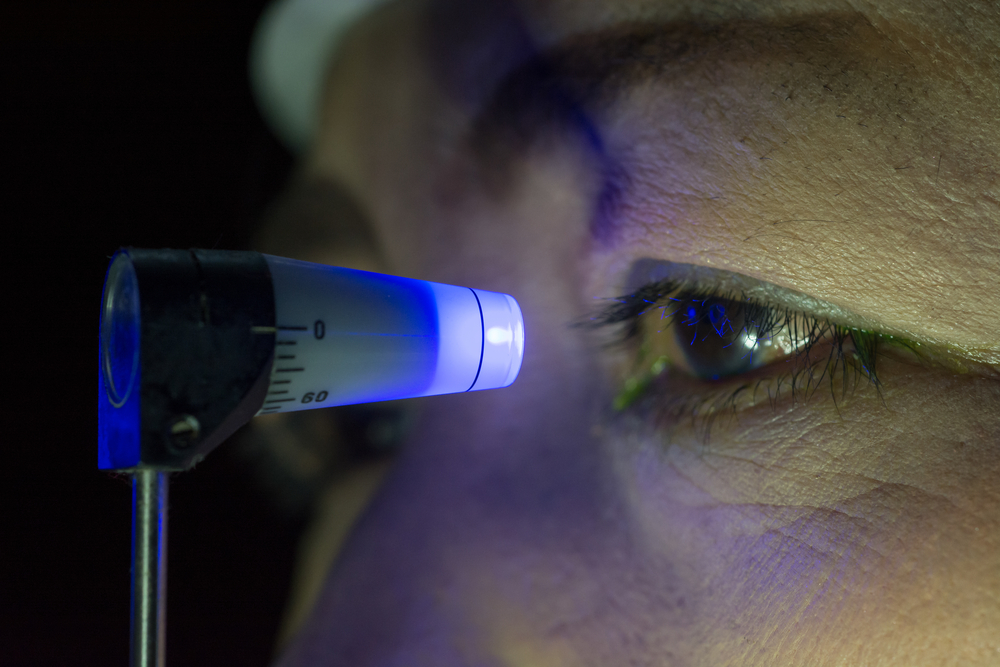
Measuring the eye pressure, or intraocular pressure (IOP). There are different ways of measuring IOP – one of the most common methods used in clinic is Goldman applanation, which involves resting a small prism on the surface of the eye after numbing drops have been applied.
Corneal thickness measurement – having a thinner cornea is considered to be a risk factor for glaucoma and having an especially thin or thick cornea can effect the accuracy of the IOP measurement.
Gonioscopy – this refers to inspection of the drainage space (angle) of the eye and involves gently resting a lens on the surface of the eye after numbing drops have been applied. This test identifies any abnormalities of the angle which may be contributing to glaucoma.
Visual field analysis – this is test identifies areas in the vision which have been damaged through glaucoma. The test involves fixating on a central target whist test lights are presented in different parts of the visual field. Each eye is tested separately.
Optical coherence tomography (OCT) – this measures the thickness of various layers at the back of the eye which are known to become thinner in glaucoma
Can glaucoma be treated?
At present, most treatment for glaucoma is aimed at reducing the eye pressure. By doing so, the rate at which glaucoma progresses can be slowed down or stabilized.
The 3 main classes of treatment are
- eye drops
- laser treatment
- surgery
Your eye doctor can advise you on risks and benefits of each option as well as advising on the best option once a thorough assessment has been carried out.